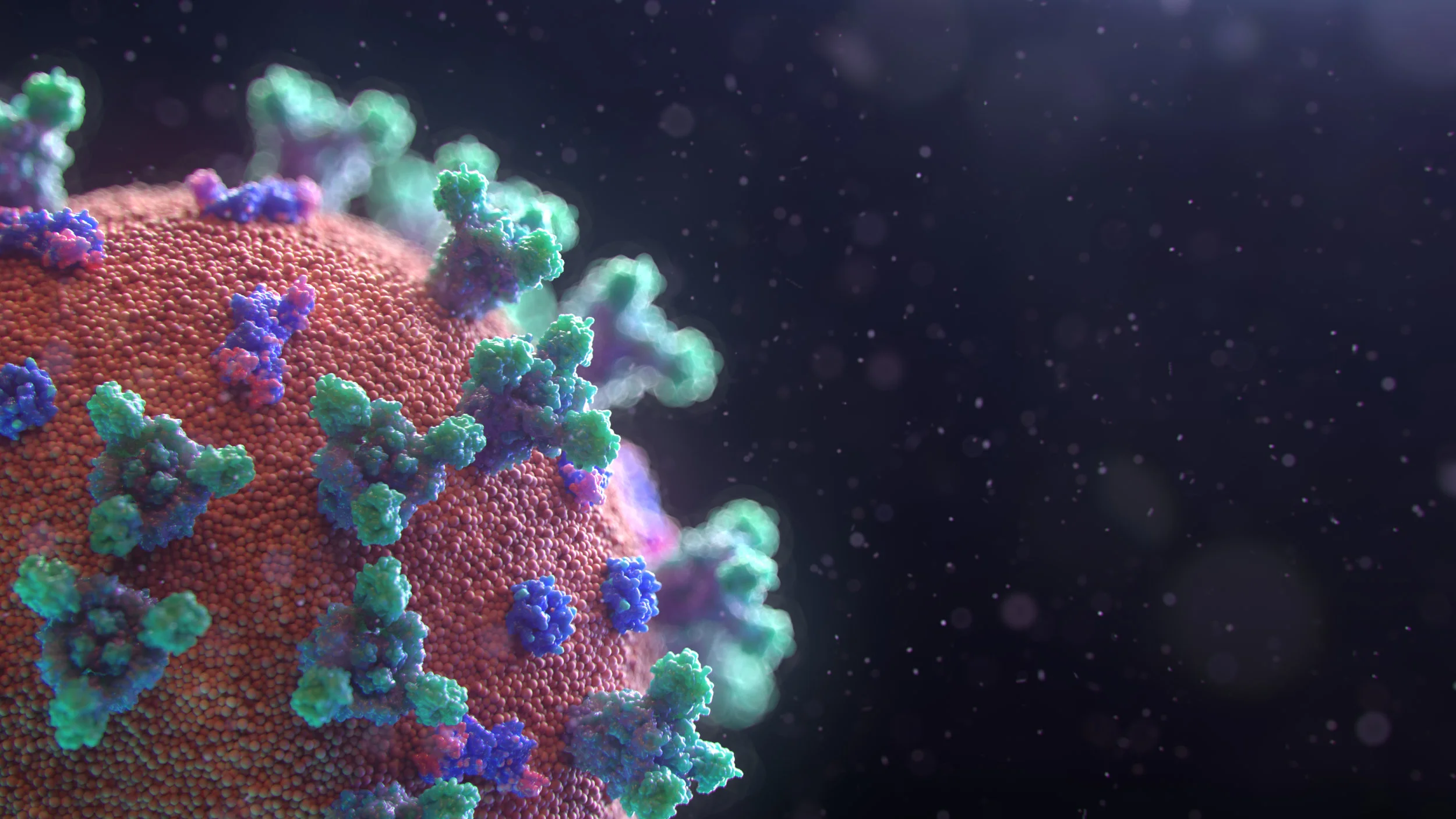
With the all talk of antigen tests, antibodies, cytokine storm and so on surrounding coronavirus, I thought it could be useful to give you a brief primer on the immune system. Immunology has been a special interest of mine since I did my first degree back in the early 1980s and my PhD was in immunology, so I have been particularly interested in how coronavirus interacts with the immune system. In this two-part article I will show you how our immune systems respond to infection.
While there has been much talk of antibodies against coronavirus, the first line of the body’s defence is nothing so specific as antibodies.
Physical barriers
Immune defence starts with physical barriers to infection (e.g. the skin, gut lining), and is enhanced by antimicrobial chemicals secreted in the saliva and tears, and the acid in our stomachs. All our internal surfaces that are exposed to the environment (i.e. our lungs and airways, and the gut lining) are coated with mucus that is able to trap potential infectants and these surfaces also support a large population of friendly bacteria that can attack potential pathogens (a pathogen is any disease-causing organism) or at least compete with them to prevent them from setting up home.
Innate immune system
If an infective agent manages to evade the physical and chemical barriers, the next line of attack is the innate immune system. This uses certain ‘hard-wired’ strategies to provide a rapid, general, response when alerted by certain typical signals of infection or tissue damage (these are called pathogen-associated molecular patterns or damage-associated molecular patterns: also known as PAMPs and DAMPs).
Dendritic cells, macrophages and neutrophils wait behind the walls of the small intestine
Tissues such as the skin, mucosal surfaces, gut and airways contain populations of immune cells (dendritic cells, mast cells and basophils) whose job is to act as sentinels for infection or tissue damage. These sentinels respond to PAMPs and DAMPs by triggering inflammation. The purpose of inflammation is to cause a chain of reactions that send out calls for specialised immune cells to come to the area of infection or damage and increases the blood flow to the area in order to enable these reinforcements to arrive in large numbers. This increase in blood flow results in the redness, heat and swelling that is so typical of inflammation. The sentinel cells use chemical messengers called cytokines to send out their calls for help.
These cytokines attract immune cells that can seek out and engulf bacteria, virus-infected cells or any damaged cells or parts of cells due to tissue damage (e.g., if you bruise yourself, twist your ankle or just wear and tear on the body). The cells of the innate immune system responsible for killing infections are neutrophils, macrophages and natural killer (NK) cells. NK cells are especially used to kill virus infected cells. The first cells to arrive are the neutrophils. Neutrophils can detect PAMPs and DAMPs and not only make the danger safe by engulfing bacteria and virus-infected cells but also contain powerful chemicals that destroy them. The neutrophils in turn release cytokines that recruit further immune cells and also increase inflammation.
Another arm of the innate immune system is the complement system. It consists of a series of proteins (found in solution in the blood) that can interact with bacteria or virus-infected human cells. Triggered by PAMPs, once activated, the complement proteins assemble to form complex structures on the surface of microbes that punch holes in the membrane thus destroying the cells. The complement system also attracts neutrophils which then eat up the complement-destroyed cells.
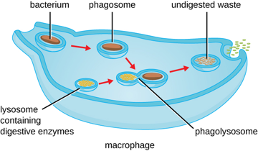
A macrophage ingests a bacterium, kills and digests it
Once neutrophils have ingested pathogens or damaged cells, they do not live for long. It is important that, before they die, they and their load of engulfed PAMPs and DAMPs and powerful antimicrobial chemicals, are in turn neutralised by another immune cell, the macrophage. Macrophages are next to arrive at the site of infection (or tissue damage). They not only process dying neutrophils and independently engulf pathogens but also initiate repair processes via anti-inflammatory cytokines and other factors. If the macrophages are unable to cope with the burden of pathogens/dying neutrophils, they recruit more immune cells and inflammation increases. Thus, neutrophils and macrophages work together to enhance the immune response against pathogens but at the same time this relationship needs to be tightly regulated as it may cause inflammation to continue and become out of control rather than resolve. When inflammation at a low level (chronic inflammation) it can cause a variety of chronic conditions. If inflammation continues to ramp up out of control and more and more cytokines are produced to recruit more immune cells, the release of the neutrophils’ killing chemicals start to damage tissues and we get a situation of runaway inflammation and the so-called “cytokine storm” that appears to be behind severe reactions to coronavirus.
The innate immune system gets to work very rapidly: within hours of infection. However, it has no “memory” and, therefore, it is unable to recognize the same pathogen should the body be exposed to it in the future. This is the function of the adaptive immune system, which I will cover in part 2.
Nutritional considerations
Before you move to part 2, I want to tell you a bit about how nutrition can affect the innate immune system.
The first, physical barrier to infection relies on the nutrients needed to create good quality skin, mucous membranes, enzymes and gut health. These are vitamins A, C, D, B6, B12 and folate; zinc, iron, copper and selenium; collagen and glutamine.
For neutrophils and other cells that destroy pathogens to be able to make their toxic chemicals, they need vitamins C and E; zinc, iron, copper, selenium and magnesium.
To allow immune cells to multiply, to migrate to the area of infection and produce their cytokines we need vitamins A, C, D, E, B6, B12 and folate; zinc, iron, copper, selenium and magnesium.
Certain nutrients are essential for both the triggering of the acute inflammation which is needed to recruit immune cells but also for the repair functions initiated by macrophages once the need for inflammation is over. Vitamins A, C, E and B6; potassium, zinc, iron, copper, selenium and magnesium are all involved in regulation of inflammation. The essential fatty acids are also closely involved in regulation of inflammation and especially in resolution of inflammation.
PAMPs are also found in certain types of food. For example, foods that have been chopped or minced which allows a big surface area for bacteria to multiply have been shown to contain PAMPs that are recognised by the innate immune system. This is one reason why foods are better prepared as fresh as possible: don’t buy pre-sliced vegetables or keep minced meat in the fridge for long before cooking.
High blood sugar can adversely affect many aspects of the innate immune system, including neutrophil function, complement function and anti-inflammatory cytokines. A good reason to avoid spiking your blood sugar with high carb/high sugar foods!
As you can see, eating a diet rich in essential nutrients is important to ensure your immune system can act quickly to protect yourself from invaders.
In the next in this series, I look at the next, more sophisticated system that our immune systems bring to bear to protect us both in the short-term but in the long-term too.
If you are feeling that your immune system could do with some support, please do contact me to discuss how my programs of nutritional therapy can help.